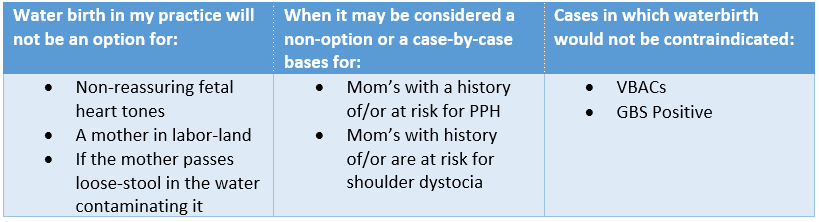
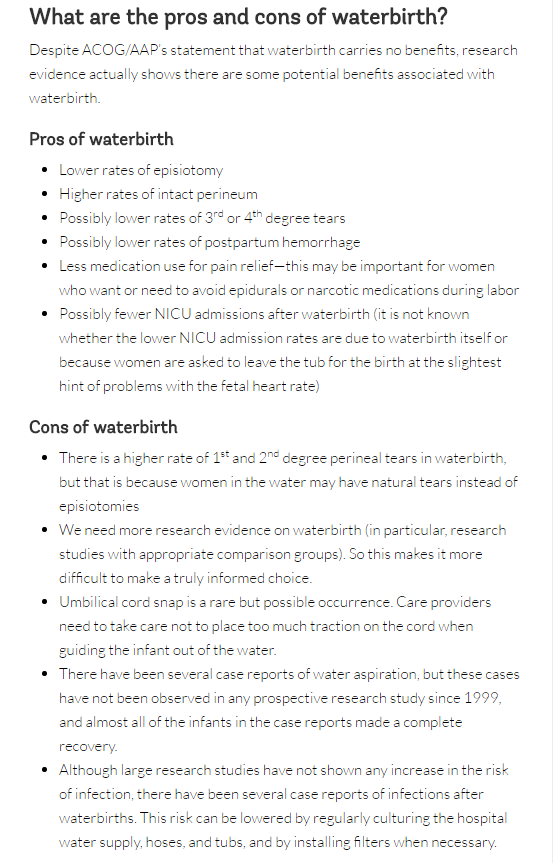
 Happy mom with her healthy baby minutes after delivering in a birth pool at home. Happy mom with her healthy baby minutes after delivering in a birth pool at home. The practice of waterbirth has always been, to me, the equivalent of a mother choosing which position she desired to labor in. I had not realized until I became a student midwife that not only was there additional benefits to choosing it, but that there is also some opposition against it. Naturally, as a student, I was intrigued to learn what the known benefits and risks are, and why is there opposition against choosing waterbirth. I started my research by reading the American congress of obstetricians and gynecologists (ACOG) committee opinion on what they referred to as “Immersion in Water During Labor and Delivery” aka waterbirth. Of course, I read it with my water birth experience in mind, so I was finding it very interesting that the complications ACOG was referring to occurring more during waterbirths, I had yet to experience. Although their evidence was very slim, they explained their findings in a way that suggested care providers avoid waterbirth. Still, even ACOG had to admit that “There are insufficient data on which to draw conclusions regarding the relative benefits and risks of immersion in water during the second stage of labor and delivery.” Still they continue with “Therefore, until such data are available, it is the recommendation… that birth occur on land, not in water.” So, their stance is, we cannot prove it is unsafe, but let’s not do it anyways since we didn’t see great benefits in our hospital trials. The unfortunate part, to me, about ACOG’s statement was that it would turn care providers away from offering waterbirth, and women away from choosing it. Speaking from personal experience as a doula, I had so many clients go on hospital tours in which they would be shown the bath tub and told that the hospital offered waterbirth, yet time and time again when it would come down to it, clients would have to beg the nurses to allow them into the tub, where if they were allowed, it was only for a limited amount of time and they were always told that birthing in the tub was not allowed. So, I know that even though clinical trials were done in hospitals to determine the risks and benefits of waterbirth, the hospital setting also carries a very different mindset on waterbirth which makes it difficult to accept, and therefore the care during waterbirths is different as well. A prime example of the care affecting the outcome is how ACOG referred to an increased chance of Umbilical cord avulsion (cord “snapping” or cord rupture) as the newborn is lifted or maneuvered out of the water. I see this as an increased chance in the hospital trials because the care providers are so focused on bringing the neonate out of the water quickly following the birth, that they do not take into full consideration the possibility of a short cord. I know this feeling myself, because as a beginning student, I too use to rush to bringing the neonate up immediately after the birth, which in most cases was fine, but sometimes if the neonate was tangled in its own cord I would struggle with bringing them up and then trying to unravel them without letting them become re-submerged. Thankfully my preceptor taught me patience with this and how to unravel the neonate from their cord while still submerged. Once I discovered this and became comfortable with the practice, I desired for more mothers to choose waterbirth and I found managing tangled cords was a breeze in comparison to delivering on land. Although ACOG was willing to take a step forward to consider the benefits of water birth, their research provided was quickly analyzed by the American Association of Birth Centers (AABC) and Evidence Based Birth. AABC not only analyzed the ACOG trial, but also collected their own data on waterbirth in the birth center environment. AABC’s data demonstrated that “Water birth, with careful selection criteria and experienced providers, does not negatively affect mothers or newborns…. The claim that water birth is dangerous for mothers and babies is not based on prospective population data with skilled birth attendants, but on negative outcome case reports or individual case outcomes reported in a large surveillance study from another country.” Furthermore, Evidence Based Birth went on to prove that ACOG’s evidence was not very accurate “The literature review in the opinion statement was outdated and did not reflect current evidence. Out of 29 references, only six were from the past nine years (2005 or later).” (Evidence Based Birth) With all the research taken into consideration and including my own experience, I fully plan on keeping waterbirth as part of my practice and I will continue to consider it safe for low risk mom’s and babies. Still, I do believe that having a protocol in place is best to decrease the chances of unnecessary interventions and emergencies. So, I have created my own protocols based on experience. Non-reassuring fetal heart tones:
0 Comments
Leave a Reply. |
AuthorHi, I'm Kaitlin. I love traveling and working as a midwife. These are a few of my adventures and the lessons I've learned from them, as well as lessons I'm still learning. Archives
April 2017
Categories |

 RSS Feed
RSS Feed
