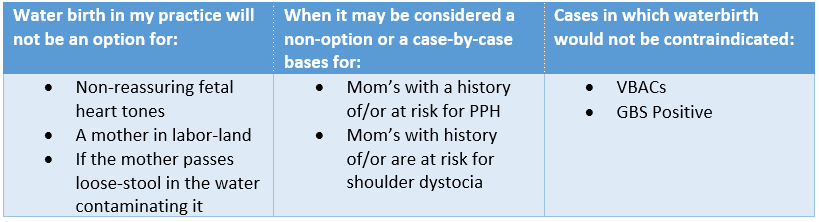
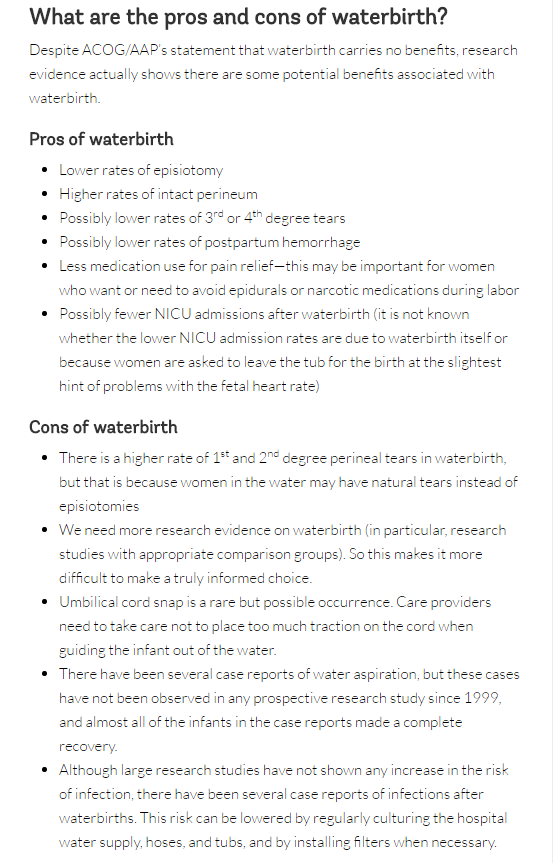
 Happy mom with her healthy baby minutes after delivering in a birth pool at home. Happy mom with her healthy baby minutes after delivering in a birth pool at home. The practice of waterbirth has always been, to me, the equivalent of a mother choosing which position she desired to labor in. I had not realized until I became a student midwife that not only was there additional benefits to choosing it, but that there is also some opposition against it. Naturally, as a student, I was intrigued to learn what the known benefits and risks are, and why is there opposition against choosing waterbirth. I started my research by reading the American congress of obstetricians and gynecologists (ACOG) committee opinion on what they referred to as “Immersion in Water During Labor and Delivery” aka waterbirth. Of course, I read it with my water birth experience in mind, so I was finding it very interesting that the complications ACOG was referring to occurring more during waterbirths, I had yet to experience. Although their evidence was very slim, they explained their findings in a way that suggested care providers avoid waterbirth. Still, even ACOG had to admit that “There are insufficient data on which to draw conclusions regarding the relative benefits and risks of immersion in water during the second stage of labor and delivery.” Still they continue with “Therefore, until such data are available, it is the recommendation… that birth occur on land, not in water.” So, their stance is, we cannot prove it is unsafe, but let’s not do it anyways since we didn’t see great benefits in our hospital trials. The unfortunate part, to me, about ACOG’s statement was that it would turn care providers away from offering waterbirth, and women away from choosing it. Speaking from personal experience as a doula, I had so many clients go on hospital tours in which they would be shown the bath tub and told that the hospital offered waterbirth, yet time and time again when it would come down to it, clients would have to beg the nurses to allow them into the tub, where if they were allowed, it was only for a limited amount of time and they were always told that birthing in the tub was not allowed. So, I know that even though clinical trials were done in hospitals to determine the risks and benefits of waterbirth, the hospital setting also carries a very different mindset on waterbirth which makes it difficult to accept, and therefore the care during waterbirths is different as well. A prime example of the care affecting the outcome is how ACOG referred to an increased chance of Umbilical cord avulsion (cord “snapping” or cord rupture) as the newborn is lifted or maneuvered out of the water. I see this as an increased chance in the hospital trials because the care providers are so focused on bringing the neonate out of the water quickly following the birth, that they do not take into full consideration the possibility of a short cord. I know this feeling myself, because as a beginning student, I too use to rush to bringing the neonate up immediately after the birth, which in most cases was fine, but sometimes if the neonate was tangled in its own cord I would struggle with bringing them up and then trying to unravel them without letting them become re-submerged. Thankfully my preceptor taught me patience with this and how to unravel the neonate from their cord while still submerged. Once I discovered this and became comfortable with the practice, I desired for more mothers to choose waterbirth and I found managing tangled cords was a breeze in comparison to delivering on land. Although ACOG was willing to take a step forward to consider the benefits of water birth, their research provided was quickly analyzed by the American Association of Birth Centers (AABC) and Evidence Based Birth. AABC not only analyzed the ACOG trial, but also collected their own data on waterbirth in the birth center environment. AABC’s data demonstrated that “Water birth, with careful selection criteria and experienced providers, does not negatively affect mothers or newborns…. The claim that water birth is dangerous for mothers and babies is not based on prospective population data with skilled birth attendants, but on negative outcome case reports or individual case outcomes reported in a large surveillance study from another country.” Furthermore, Evidence Based Birth went on to prove that ACOG’s evidence was not very accurate “The literature review in the opinion statement was outdated and did not reflect current evidence. Out of 29 references, only six were from the past nine years (2005 or later).” (Evidence Based Birth) With all the research taken into consideration and including my own experience, I fully plan on keeping waterbirth as part of my practice and I will continue to consider it safe for low risk mom’s and babies. Still, I do believe that having a protocol in place is best to decrease the chances of unnecessary interventions and emergencies. So, I have created my own protocols based on experience. Non-reassuring fetal heart tones:
0 Comments
It has been over three and a half years since I wrote the first part of this blog. By now the memories of my last days in India somewhat blur together, but the memory of this one story stays with me as strong as ever. It is the story of Jina.
------------------------------------------------------------------------------------------------------------------------------------------------------------------ I pried my fingers from the grieving mother I was with because another mother was being placed on the empty metal bed next to her. Normally I wouldn't leave one women for another so quickly, most of all one who just lost her baby, but this new mother was seizing and I was needed to help hold her down. She was so young; her baby bump was very elongated and easy to hide behind a sari, which was surprising for her small figure. As I held her down her skin felt to me hotter than the temperature of the day, which was exactly the case. Her seizure was being caused by a fever of 106.2 F. As she was held down by my instructor, Rachel, and I, we called to the doctors for some medications to bring down the fever, but the doctors ignored our calls in the misted of the chaos. After the mothers seizure ended Rachel left me and another student, Lindsay, to care for the mom as she went to get the needed medications herself. The mother was unconscious at this time, so I left as well to gather up some cleaning rags and hand washing bowl. I rinsed out the bowl and rags as best as could before filling it with new water. I rushed back to the moms side where Lindsay and I starting placing the few rags over the mom as best we could. It was at this time that we noticed the moms belly was tightening, and then relaxing… she was in labor. Rachel returned and administered the medications as we let her know that the mother was in labor. So she slipped on a glove and checked the mother for dilation, she was a full 10cm! I immediately checked for the baby’s heartbeat. After a quick palpation and some moving around of the pinard, I heard the sweetest sound, the song to midwives ears; a strong heartbeat! As I lightly nodded my head to the beat while watching the seconds of my watch tick, my excitement changed. The baby’s heart rate was pushing 176 BPM. If this baby was going to have any chance it needed to come out now! But with an unconscious mother, no amount of fundal pressure was going to get the baby out soon enough. Rachel grabbed the attention of one of the doctors and upon explaining the situation asked the doctor to please bring the forceps and deliver the baby. The doctor looked at all of us trying so hard to help this one woman and said to us “Look, this is a waste of your time. This girl is 17 and no one in her family knows she is even pregnant. She lives alone with her father as her mother passed away many years ago. Her father will beat her if she returns home with a baby. She is better off if the baby dies.” We didn’t become upset with the doctor because we knew too well how this was normal for their culture, but we also were not going to let the culture be the reason why the baby lost its life. So we didn’t give up. Rachel asked every doctor there, she even asked to perform the forceps delivery herself. Meanwhile she continued to find medications as needed, and I continued to refresh the water and rags as much as possible as Lindsay stayed by to help among helping as many other women as possible. One hour went by... Her temperature had dropped to 105.4 F and the fetal heart rate was 172 BPM. Another hour... Temp was now 104.8 F, fetal HR was 168 BPM Another hour... Temp: 104.2 F, FHR: 132, Mother was still unconscious. After three full hours we had not left her side. There was so much work to be done that Rachel convinced the first doctor we asked that if she would just deliver the baby that we would move on to help with other things. So the doctor agreed to help us. After all, if the baby was still alive after this long there may be a better chance of survival than she had originally assumed. In preparation of this forced delivery we all gathered around and positioned ourselves so that we could hold the mother in place, pull back her legs and apply fundal pressure all on the doctor’s command. Before beginning, the doctor reached inside the mother to manually break the bag of waters. As the bag of waters broke the doctor yanked back her hand and started shaking it as if she had just touched a hot stove. The yank of her hand was followed by a think yellow fluid that steamed as it spilled onto the metal bed; meconium. FRH: 122… and dropping fast. Through a mass amount of teamwork the mother was pushed and pulled until the doctor was able to bring out a beautiful baby girl with a head full of dark dreamy Indian hair. I took one look at her and called her Jina. The name Jina had two meanings. In Tanzania Jina meant Name, and in India I leaned from one of the nurses that it meant Loved. If anyone deserved to be loved and given a name, it was this little girl. We cleaned her and suctioned her as best we could, but her heart rate was now only 96 and her limp body refused to breath. Rachel and I immediately began CPR as we prayed over and over for the life of Jina. Her heat rate continued to drop as her unconscious mother was being stitched up. After five minutes of CPR Jina’s heart was now beating at only 60 BMP. By 10 minutes, only 30 BMP. At that moment the cleaning lady came in and motioned for us to give her the baby. As Rachel handed her Jina she explained that the baby was still alive and that it needed to be taken to the NICU; which in this case was a long walk up three stories and on the other side of the hospital. The cleaning lady bobbled her head and giggled at us -as they often did because she most likely didn’t understand a word we said but found our American ways funny-. She walked out of the ward with Jina held up over her shoulder in one hand and a bucket of cleaning supplies in the other. I never saw either of them again. The mother was cleaned up and left alone as we went on about finishing up our work for the afternoon. In just a short while the workload slowed and it was time for everyone in our group to leave. As our last day at the hospital; we never saw the mother regain consciousness, and although presumed dead, I never saw Jina again. I couldn’t imagine what it would be like for the young mother to wake up. One moment hiding a pregnancy, the next moment waking up in pain, without so much as one look at her baby. Whether she wanted the baby or not, I knew there would be no support for her. No one to tell her what happened, and no one to tell her how beautiful Jina was. Had Jina survived and the mother been conscious, and still not wanted her, I would have certainly adopted her. I often dream of what my life would like today if I had a beautiful little girl from India who would soon be turning four years old. The story of Jina doesn’t stay with me because it was tragic; it stays with me because it reminds me every day of what God has created me to do. To love those who may not understand love and to fight for those who cannot fight. What I once thought would go on forever, ended almost as suddenly as this very second, or so it felt. Now: Each day gives reality the weight needed to sink deeper and deeper into my heart, and it manages to find places so dark I nearly lose myself in it many times. To sit down and think about one's life is a challenge, to think about the lives you have changed is greater yet, but to sit down and realize the lives that have changed yours, well that, for me, has been life changing.
Each day was so different, yet looking back they all blur themselves together, as if it were all just a dream. You wake up to find the people that were in the dream are nowhere around, and those who are now around you seem only to be happy that you are awake. But in those fine moments of awakening, you can't help but wonder, “Was I really dreaming? Or was my dreaming really real!?” It was our last day in the hospital, and I was assigned to the admissions ward. Work was hit and miss with the admissions ward, some days you never sat down, other days it seemed sitting was all there was to be done, but this day was different, it was like one of those sweltering summer days that begs to differ the very existence of snow ever falling on the same land. The thought of having nothing to do on this day laid only in the minds of those who could not think. Multiple women on beds, many on the floor, and more were coming in. The few doctors there looked like octopuses, in my mind, as they were moving so fast I could hardly count the amount of hands they actually had. Young student nurses ran around busy as ever but always seemed to have the “deer in the headlights” look about them as they had almost no supervision and nearly everything they were doing, they were doing for the first time. We stepped into the middle of it all. Those of us, who were not taking orders from the doctors, were giving orders to the student nurses. With just a few moments to asset each situation I managed to work my way towards the examination room. I pulled the green stained curtains back just enough to get in and asset any situations inside. Two metals beds, one empty, the other with a mother lying alone. I first saw her eyes, they were dark and distant. She stared at the wall continuously as if I hadn't even entered. I followed her eyes down, her sari modestly covered her chest, but her legs were open and bare for the world to see. And there, just next to me, a site I had seen too many times before. A baby, a little girl, tiny, limp, macerated. Lying in her mother’s fluids, and alongside her a placenta as black as death itself. I'm sure the mother was waiting for me to slap her around and sweep the baby away just to get her out of the room to make way for the multitude of women in waiting. But no, I ran to her side and grabbed up her hands in mine. We didn't share the same language, but I spoke anyways. I prayed. She had no idea what I was saying, no idea who I even was, we were strangers in every way, yet after just a few words, she clang to me. She gripped my hands tighter and tighter with every word, and then she cried. She didn't dare let me go, even as I checked her vitals. And I was with her as we watched a cleaning lady put on one glove, and toss the baby into a cardboard box as if it were meat to go out to the trash. I ran my fingers through her hair, gave her a kiss on the forehead and then with one last prayer I pried her fingers from me, and walked away. Back to my duties, for I had only been there twenty minutes…. To be continued. |
AuthorHi, I'm Kaitlin. I love traveling and working as a midwife. These are a few of my adventures and the lessons I've learned from them, as well as lessons I'm still learning. Archives
April 2017
Categories |





 RSS Feed
RSS Feed
